Reducing the carbon footprint of anaesthetic gasses
In November 2017, HCWH Europe introduced the project Fostering low-carbon healthcare in Europe for measuring hospitals’ carbon footprint, including greenhouse gas (GHG) emissions from the use of anaesthetic gases. As part of the initial workshop hosted in Bonn, participants were presented with the topic: Reducing the carbon footprint of anaesthetic gasses.
The following video is a recording of the presentation given by Dr JMT Pierce - the Environment and Sustainability Advisor at the Royal College of Anaesthetists (RCoA - UK) and Consultant Anaesthetist for the University Hospital Southampton (UK).
Dr. Pierce introduces the basics of anaesthesia and atmospheric science, and reviews the carbon footprint of agents and components used in inhalational anaesthesia (a common form of general anaesthetic), and assesses practices that can reduce this footprint.
Presentation slides available here
Various components in the anaesthesia process contribute to the carbon footprint of the healthcare sector: disposable plastic components (commonly PVC) are often combusted, with 1kg of PVC producing 3kg of CO2e. Leftover residues of intravenous drugs and some packaging materials are also combusted, whilst the inhalational agents and exhaled into the atmosphere.
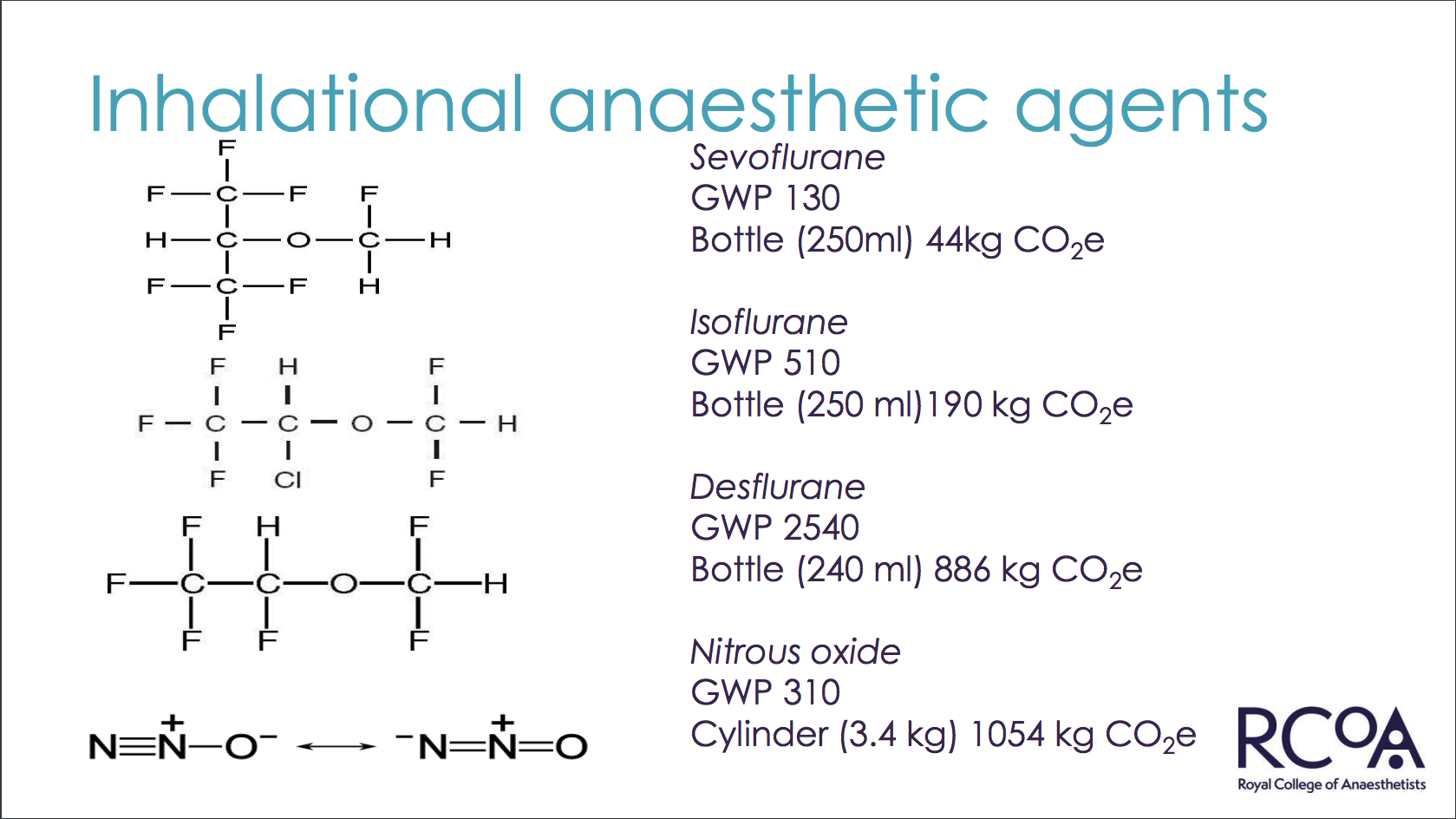
Dr. Pierce’s presentation shows the varying global warming potential (GWP) of inhalational agents, for example Sevoflurane has a GWP of 130, whilst Desflurane’s GWP is 2540 – in reality this produces a difference of over 800kg of CO2e when using small quantities of the agent (250ml and 240ml respectively).
The atmospheric concentration of inhalational anaesthetic agents has shown to be increasing over time, exacerbated by rising popularity of using agents with longer atmospheric lifetimes, which, in turn, have a greater global warming potential. In this video, Dr. Pierce explains how the inhalational agents are disgorged as CO2e during the anaesthesia process and how this is contributing to a large carbon footprint of healthcare.
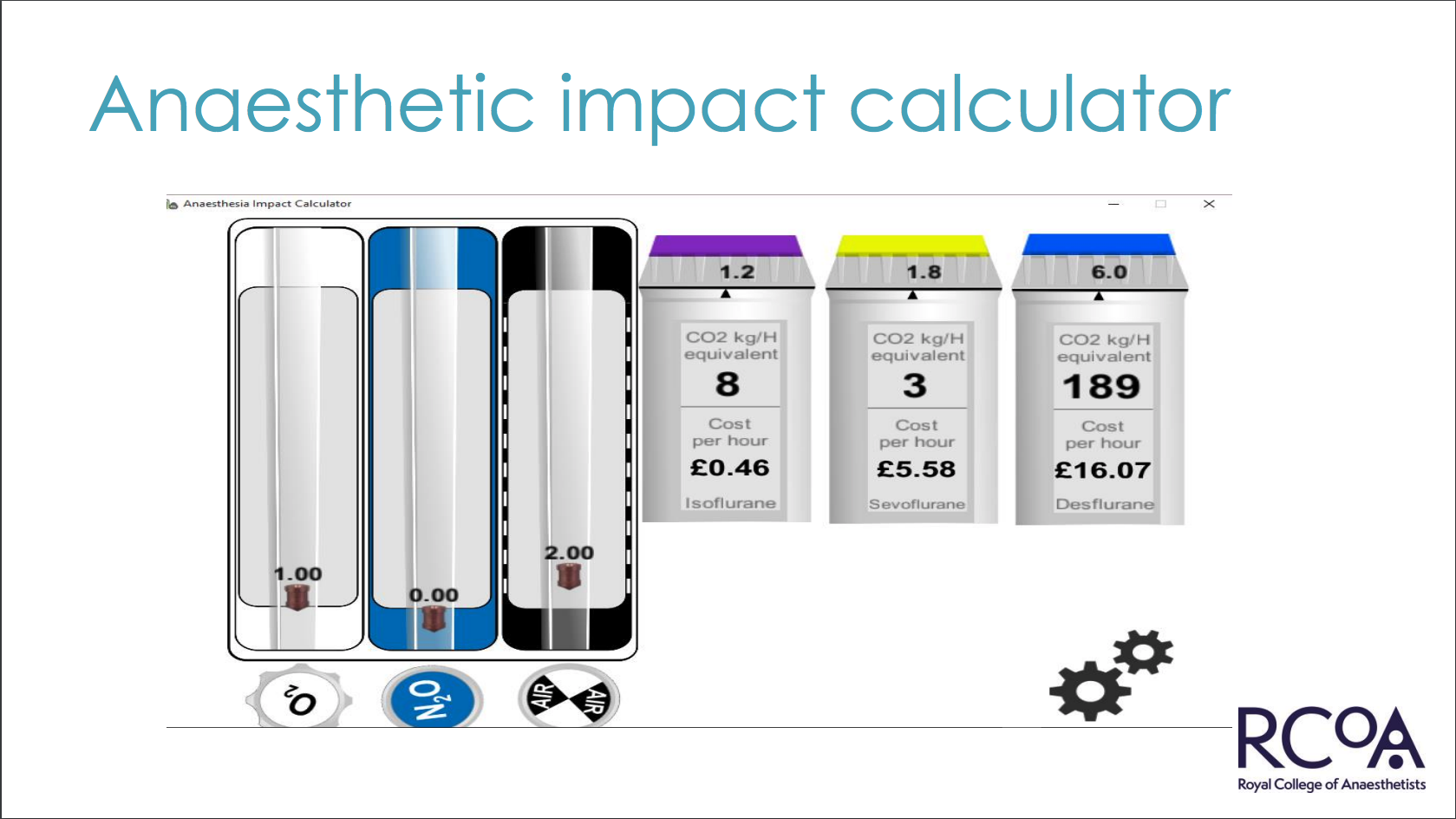
Using a real time CO2e calculator developed by the RCoA, Dr. Pierce demonstrates how simply choosing different combinations of inhalational agents and carrier gasses: oxygen (O2) and nitrous oxide (N2O) or air can greatly affect the CO2e output and cost of the anaesthesia process. In one example, simply choosing a different combination of carrier gasses yielded a 5x difference in CO2e produced. The anaesthetic impact calculator is available to download freely on iOS and Android devices.
Reducing the carbon footprint of anaesthetic gasses
Dr. Pierce closes his presentation with some examples of best practice that can help reduce the CO2e output of the anaesthesia process – from choosing different combinations of inhalational agents and carrier gasses, or simply turning off equipment when not in use. Dr. Pierce also shares some examples of quality standards for anaesthesia including from the RCoA and NHS improvement.
Dr. Pierce's presentation slides from the workshop are available here: ![]() - Reducing the carbon footprint of anaesthetic gasses - 10/11/2017.
- Reducing the carbon footprint of anaesthetic gasses - 10/11/2017.
HCWH Europe gratefully acknowledges the financial support of the European Commission (EC), the European Climate Initiative (EUKI), and the Federal Ministry for the Environment, Nature, Conservation, Building and Nuclear Safety (BMUB).
HCWH Europe is solely responsible for the content of this presentation and related materials - the views expressed do not reflect the official views of the EC, EUKI, or BMUB.